Digital Health Leadership and Strategic Management in Public Healthcare HCLD7025
- Subject Code :
HCLD7025
Part A Background Information
The Department of Health in Western Australia is a primary service agency providing health services to the state and has the responsibility of managing public hospitals, community services, and health promotion programs. It lies at the heart of policy formulation and implementation that ensures the health and well-being of WA's 2.7 million people according to the 2021 census (Australian Bureau of Statistics, 2022). It operates under the larger context of the Australian health system but primarily operates on the needs peculiar to the state's diverse population particularly those in remote and Indigenous communities.
Founded on a mission to ensure equitable access to quality health care, improvement of health, and sustainability of health systems timely and responsive, the organisation upholds values that include compassion, respect, collaboration, and accountability. With a vision to focus on promoting health, preventing diseases, integrating digital innovations into the improved outcomes of patient care, and having efficiency in service delivery, the WA Department of Health strives to achieve this end (Government of Western Australia Department of Health 2023).
This department's strategic direction is underpinned by the WA Health Digital Strategy 2020-2030, which sets a connected health system that will exploit technology for improved patient care, better decision-making, and efficient operations. It places significant stress on the ethical use of health data, on cybersecurity, and the final goal of achieving interoperability among different digital health platforms. It is aligned with the international move toward digitising health services that improve access and outcomes, which is especially relevant for the dispersed population of WA (Government of Western Australia Department of Health 2020).
The Department of Health in WA has faced various challenges in recent years, including budget pressures, an ageing population, and increased demand for services, mainly within the rural and remote contexts (Government of Western Australia Department of Health 2024a) There is also an imperative to change the healthcare system to make it more responsive and compatible with the rapid changes in technology.
The Department of Health has encountered different challenges, including budget pressures, an ageing population, and increased demand for services, primarily in rural and remote contexts. There is also a requirement to transform the healthcare system so as to keep pace with rapid changes in technology. The COVID-19 pandemic brought to the fore the need for a more robust digital health system and renewed investment in telehealth services and electronic medical records (Government of Western Australia Department of Health 2020). However, these advances also create new challenges, including meeting patients' expectations for data security, managing change due to digital transformation, and incorporating those into existing healthcare infrastructure.
The current leadership, led by Director General Dr D J Russell-Weisz, has solid backgrounds in both clinical practice and healthcare administration, and a shared aspiration to drive forward the digital health agenda (Western Australia Government, 2023). The gap created by this Executive Director Digital Health position may be interpreted as an organisation embarking towards accelerating these digital initiatives. By the way, this role nature would work through changing large-scale complexities to ensure they are aligned with the overarching goals of the department and then building partnerships with key stakeholders such as clinical staff, governmental agencies, and technology providers.
Applying for this Executive Director Digital Health position will allow me to contribute toward meaningful reforms in health care through digital innovation. I will be zeroing in on a model of patient-centered care with a sharp focus on data-driven decision-making and the most robust cybersecurity frameworks. Indeed, my experience in leadership for digital transformation and strategic relationship building equips me to face the challenges ahead.
Part B: Plan Demonstrating Healthcare and Digital Leadership
Introduction to Leadership in a Healthcare Context
Leadership in health care would be fundamental in delivering service and improving patient outcomes if ever. Good healthcare leaders not only manage their workforce but, through strategic visioning, decision-making, and partnerships, also shape the broader healthcare environment. The Executive Director of Digital Health at the WA Department of Health requires leadership related to the WA Health Digital Strategy 2020-2030. Its main aim is to push through digital health to advance patient care, secure data, and interoperability (Government of Western Australia Department of Health 2020).
Healthcare management theories refer to transformational theory and servant leadership theory, which offer simple frameworks under which complex health systems can be managed (Saleem et al., 2020). These entail patient, staff, and organisation needs. These are tailor-made for healthcare settings, and there is the LEADS in a Caring Environment, which itself has been designed to offer a structure for leadership. There is a need for strategic planning and resource alignment, and the adaptability of theories acts as a set of keys to achieving success in digital health leadership (White et al., 2023).
Strategic management calls for healthcare leaders to pay attention to long-term planning in the effective use of resources and the capacity to adapt to this rapidly changing digital health landscape. By embedding these innovation and promoting research, leaders will ensure that their teams realise better health outcomes in a dynamic ICT environment integrating people, processes, and technology (Zhang, Gong, and Zhang, 2022).
Key Selection Criteria 1. Leadership in Strategic Direction and Implementation of WA Health Digital Strategy 2020-2030
The first key selection criterion relates to leading the strategic direction and undertaking the implementation of the WA Health Digital Strategy 2020-2030, which encapsulates a holistic plan for health services to undergo digital transformation (Government of Western Australia Department of Health 2020). This reflects the leadership capacity to lead the organisation through a substantive change program.
Leadership Theories
Comparative Analysis Transformational leadership comes specifically into the spotlight in this context. Transformational leaders inspire and motivate teams through a shared vision, which is very important in large-scale digital health programs (Seljemo, Viksveen, and Ree, 2020). For example, according to my perspective, I'll implementing WA Health Digital Strategy requires an entire transformation in the delivery model of healthcare services, where leaders alone will set direction, but also foster innovation and collaboration. A transformational leader in this position would be applying emotional intelligence skills to become more connected with the team members, who would therefore be motivated to attain strategic objectives (Ann, 2020). Adaptive leadership theory can be very instrumental when it comes to the complications of digital transformation. Adaptive leaders focus on helping determine problems, mobilising people, and adjusting to the change of challenges over time (McKimm et al., 2022). For healthcare, this means responsiveness to new technologies and the evolving needs of patients and healthcare providers. According to me as an Executive Director of Digital Health, adaptability in managing the shift to digital health and ensuring its successful implementation will be vital (Western Australia Government, 2023).
Key Strengths for Comparison with Health Leadership Frameworks
The LEADS in a Caring Environment framework specifies specific capabilities that healthcare leaders should have. Within the "Lead Self" and "Engage Others" domains, leadership needs to be self-aware, communicate effectively, and engage basic skills that must come in handy to lead a complex digital strategy. Innovation and change management are highlighted under the "Systems Transformation" domain-a considerable part of the whole responsibility of implementing the WA Health Digital Strategy (White et al., 2023). Using this framework, I would indicate how my leadership approach resonates with stakeholder engagement, change management, and innovation to meet this requirement (Government of Western Australia Department of Health 2020).
Comparison with Strategic Management Concepts
This means leading the implementation of a digital health strategy with long-range planning, resource alignment, and decision-making. A good leader has to ensure that all resources-financial, technological, or human-are aligned with the strategy. Analysis of risks, benefits, and outcomes constitutes this process (Silva et al., 2022). Being part of the leadership, such tools of analysis provided by strategic analysis would have been used for appraising the effects of digital health initiatives and ensuring that the set objectives of the department are realised. In addition, some facets of project management methodologies - whether Agile or Waterfall apply to the realisation of the digital strategy. Agile encourages iterative development and continuous feedback allowing the department to respond quickly to change and improve outcomes. My experience of leading cross-functional teams in an ICT environment would mean that projects were delivered on time and within budget while meeting the broader goal of the department (Zhang, Gong, and Zhang, 2022).
Key Selection Criterion 2: Building Collaborative Partnerships and Managing Strategic Relationships Across the WA Health System
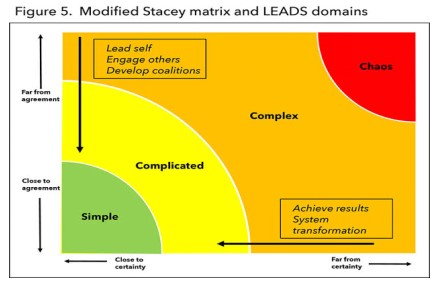
Figure 1: LEADS framework
(Source: Hartfield, 2023)
The second key selection criterion points to the building of collaborative partnerships or managing relationships with internal and external stakeholders. This plays a critical role in facilitating the effective integration of digital health initiatives across the health system.
Leadership Theories Comparison
Servant leadership is of particular relevance to this criterion. Servant leaders are concerned with the needs of members and stakeholders by soliciting trust and cooperation, in which healthcare can really work effectively to build partnerships with common goals, like improved patient care in the implementation of digital health solutions (Saleem et al., 2020). The servant leader would listen attentively to the stakeholders, empower them to contribute to the digital strategy, and ensure that their input is valued (Canavesi and Minelli, 2022). Again, here, an adaptive leader would play a strategic role in pushing for complex stakes involving relationships. Once again, adaptive leadership becomes crucial here because it is basically concerned with collaboration and, therefore, allows stakeholders to solve issues complexly (Nthel et al., 2023). If I created a collaborative and innovative space where this would be possible, I would be able to initiate some good, long-living relationships that could support the efforts for digital transformation.
Compared with the Health Leadership Framework
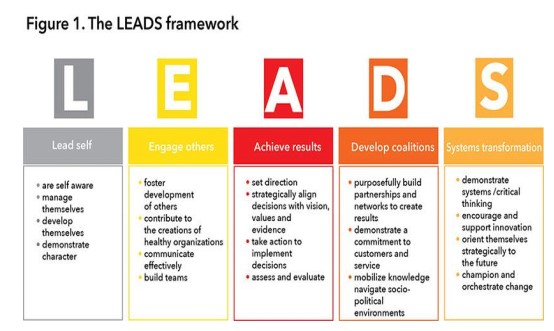
Figure 2: 5 Core Leadership Framework
(Source: Hartfield, 2023)
In the LEADS framework, one such significant capability is "Develop Coalitions," which fosters collaboration and partnership building. This capability directly relates to a requirement to lead and manage strategic relationships across the WA health system (Silva et al., 2022). Demonstrating my ability to build and maintain internal and external relationships can illustrate how I would engage stakeholders in the digital health journey. The "Lead Self" and "Engage Others" domains of LEADS, both of which are based on emotional intelligence and communication-key to develop trust and rapport with stakeholders as well as patient-centered care and strategic planning, governance, assurance, stakeholder engagement (De Brn et al., 2020).
Comparison with Strategic Management Concepts
From the point of view of strategic management, building partnerships is essential for the success of any large-scale endeavor, especially in the public health sector. The strategy involves identifying key stakeholders' needs and building them around the bigger strategy that everything points towards. In terms of the WA Health Digital Strategy, managing relationships with technology providers, healthcare professionals, and government agencies is important for ensuring the successful deployment of digital tools and systems (Government of Western Australia Department of Health 2020).
I would also use lessons from theories of relationship management, in particular stakeholder theory. This theory revolves around balancing the interests of various stakeholders (Oshni Alvandi, Bain, and Burstein, 2021). By balancing the interests of internal stakeholders - for instance, clinical staff - with those of external partners, including vendors of technology, I would be able to create a sustainable environment that fosters digital health innovation.
How Theories Fit into Selection Criteria
Both transformational and servant leadership truly align with the key selection criteria for the Executive Director of Digital Health position. Transformational leadership supports the need to set a strategic direction, inspire the team, and manage change, while servant leadership highlights relationships and collaboration (Laukka, Plkki, and Kanste, 2022). This framework of LEADS in a Caring Environment forms a robust structure in displaying how I meet the criteria, most specifically in engaging others, developing coalitions, and managing system transformations (Dickson et al., 2021). These capabilities are in line with the achievement of the WA Department of Health's goals, which hopes to deliver better health outcomes through digital transformation (Shao et al., 2022).
Adopting a holistic approach, the strategic management applied with the elements of resource alignment, risk management, and adaptability must be pursued for effective implementation of the WA Health Digital Strategy (Western Australia Government, 2023. Applying both leadership and strategic management principles could help me show a whole approach toward addressing the key selection criteria.
Conclusion
The transformational and servant leadership theories, frameworks, and strategic management concepts discussed above will provide a good foundation with which to meet the key selection criteria for the role of Executive Director of Digital Health at the WA Department of Health. Using transformational and servant leadership models, together with the LEADS framework and strategies of strategic planning in my approach, I can posit an effective communication of my ability to lead the strategic direction of digital health initiatives, build partnerships, and manage complex change programs for delivering better health outcomes for Western Australians.
C. Draft Responses to Selection Criteria
Ability to lead the overall strategic direction-setting and implementation of the initiatives outlined within the WA Health Digital Strategy 2020-2030, including the implementation of the complex change program.
Key Selection Criterion 1: Demonstrated Strong Communication and Collaboration Skills
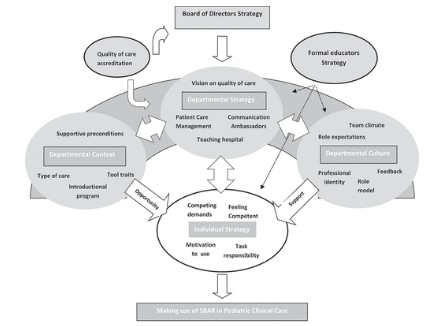
Figure3:SBAR-Situation-Background-Assessment-Recommendation Model
(Source: Coolen et al., 2020)
Good communication in healthcare is key to ensuring safe, high-quality patient care and supporting collaboration across multidisciplinary teams. In WA Health Digital Strategy 2020-2030, communication is henceforth needed to align various stakeholders like clinicians, administrators, IT specialists, and patients towards a commonly shared vision of digital transformation (Government of Western Australia Department of Health 2020). Good cooperation makes the efforts of all participants move in the same direction, which is an essential aspect of a change process as complex as this one. Last but not least, great leadership in digital health should be able to articulate clear strategic directions and collaborate with a variety of stakeholders in the health system.
From the academic texts, best practice can now come through evidence showing structured frameworks, for example, SBAR-Situation-Background-Assessment-Recommendation. According to Coolen et al., (2020) in the Journal, SBAR minimises errors, adds clarity, and ensures that important information is conveyed briefly and correctly during patient handovers also shown in the figure. Such principles of structured communication hold paramount significance when directed toward the leadership of digital health change initiatives in order to ensure alignment for the team members with the strategic direction and thus, their roles (Ruhomauly et al., 2019).
Personal Experience and Knowledge: As a healthcare team leader, in my tenure, I have used the structured communication technique in several settings. One such instance was the implementation of an EHR system. The clinical staff had resisted the change initially because they thought that the transition to the EHR system would be too much for them to handle and was not user-friendly (Dusin, Melanson, and Mische-Lawson, 2023). I organised interdepartmental training sessions wherein clinicians and IT specialists collaborated to find solutions to usability issues. I also ensured that the department's concerns are heard and addressed by the IT team through structured meetings using SBAR (Ruhomauly et al., 2019). This I was able to do through open communication and collaboration, meaning that the teams were accordingly aligned with their strategic goals and successful implementation of the EHR with the least disruption possible on patient care.
Response: In my different leadership positions, I have managed to ensure efficient communication of strategic objectives and promote team collaboration. I used structured communication while implementing the EHR. This helped ensure that all the questions of the staff members were addressed and all the stakeholders were aligned with the overall goals. I, therefore, encouraged collaboration between the teams - clinical and IT teams (Australian Commission on Safety and Quality in Health Care, 2024). The transition has been smooth until now, and patient care outcomes along with the satisfaction of the staff have improved (Zhang, Gong and Zhang, 2022). My experience in such leadership roles directly supports my capability to drive the strategic direction-setting and implementation of the WA Health Digital Strategy 2020-2030, especially in managing complex change programs (Government of Western Australia Department of Health 2020).
Key Selection Criteria 2: Problem-Solving and Decision-Making Skills
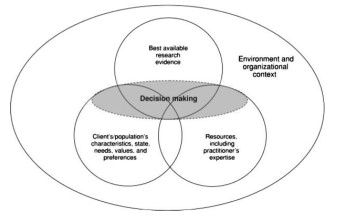
Figure 4: EBP model
(Source: Mansholt et al., 2013)
Understand how to be successful in building collaborative partnerships and managing strategic relationships across the WA health system with key internal and external stakeholders (Western Australia Government, 2023.
Understanding what is needed In health care leadership, there is the need for critical thinking for appropriate problem-solving and decision-making when working in strategic relationships and partnerships. A balance between clinical evidence, patient needs, and the limitation of resources has to be made in clinical decision-making in order to achieve the best outcome. Successful partnerships in the WA health system entail identifying and working together on potential challenges related to workflow inefficiencies, resource constraints, and stakeholder engagement (Dickson et al., 2021). It is those skills that will help drive innovation and achieve the long-term goals of the WA Health Digital Strategy.
Applying Best Practice from Scholarship: The EBP model refers to a systemic approach to making decisions in the healthcare environment. EBP combines, where appropriate, the best available clinical evidence with information about the patient's unique clinical course, for individualising decision-making, assured to be patient-centered and evidence-based(Australian Commission on Safety and Quality in Health Care, 2024). Research by Melnyk and Fineout-Overholt highlights the significance of EBP in enhancing patient outcomes and effectiveness in healthcare (Dusin, Melanson, and Mische-Lawson, 2023). Similarly, strategic decision-making models exist like SWOT, whereby a specific organisation determines its Strengths, Weaknesses, Opportunities, and Threats, thus engaging in concrete steps toward finding the solution and making the right decisions.
Personal Experience and Knowledge: In the previous organisation, one of my responsibilities involved concern over late discharge from the health facility, which resulted in both low patient satisfaction and inefficient utilisation of facilities. Through the EBP model, I collected data concerning the times taken before discharge, when the workflow was inefficient, and feedback from patients (Dusin, Melanson, and Mische-Lawson, 2023). I analysed the SWOT to establish strengths in the care given but identified weaknesses in communication between departments (Shao et al., 2022). There were opportunities to improve: streamlining processes in discharge planning would benefit the organization, and the growing threat of increasing patient dissatisfaction was a pressing need.
Response: Armed with these learnings, I developed several new modifications: a new coordinated care protocol integrating automated notifications within the EHR system. All departments were then immediately aware of when patients were ready for discharge, thereby greatly reducing delays in communication. Consequently, discharges decreased by 20%, and patient satisfaction improved significantly while releasing hospital resources more effectively (Dusin, Melanson, and Mische-Lawson, 2023).
Evidence-Based Approach: I have always ensured evidence-based approaches and structured decision-making models in response to very complex healthcare problems. The reduction in delays that preceded the patient's discharge best proves my capacity for identifying problems, analysing data, and effecting solutions that have improved both care outcomes and operational efficiency (Shao et al., 2022). My experiences in managing internal partnerships between clinical and administrative teams also support this because they demonstrate my capacity to build collaborative relationships that drive system-wide improvements.
Example: I instituted a strategic partnership between the hospital I represented and the local health IT provider for this new patient monitoring system. This ensured constant communications and coordinated the interests of internal stakeholders (both clinicians and administrators) with those of external partners (IT providers), so that the project did not derail but delivered the expected outcomes. It assured more modern and enhanced capabilities in patient monitoring and brought out better safety and quality care for patients across the entire hospital.
My communication, collaboration, problem-solving, and decision-making skills are very well lined up with the requirements in the WA Health Digital Strategy 2020-2030. I was able to lead teams with success and manage partnerships by structuring formal communication and making decisions that were based on evidence, with dramatic improvement in delivering healthcare (Government of Western Australia Department of Health 2020). I am confident that these skills will be able to support such strategic initiatives arising from the WA Health Digital Strategy as it shapes innovation and drives improvements in health outcomes across the system.
D Career Pathway: Steps to Complete the Plan
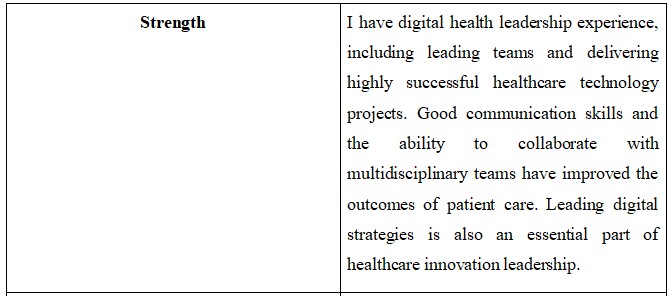
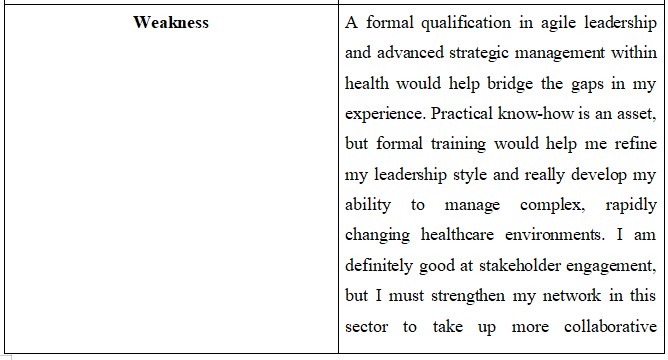
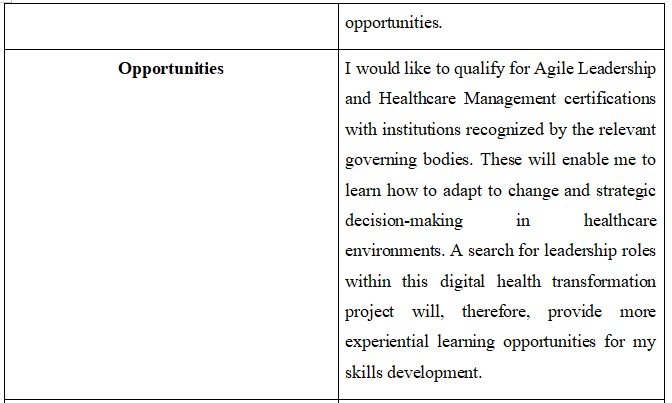
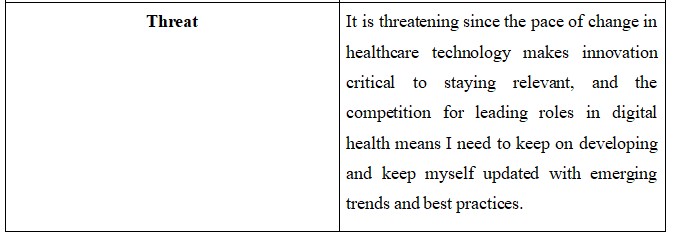
As I continue growing in healthcare leadership, some of the important skills to be acquired include agile leadership, strategic thinking, communication, and problem-solving. A SWOT analysis will be used to determine the strengths and weaknesses capabilities in order to plan the right next steps.
SWOT Analysis
Table 1: SWOT Analysis
Action Plan for Growth
Table 2: Action Growth Plan
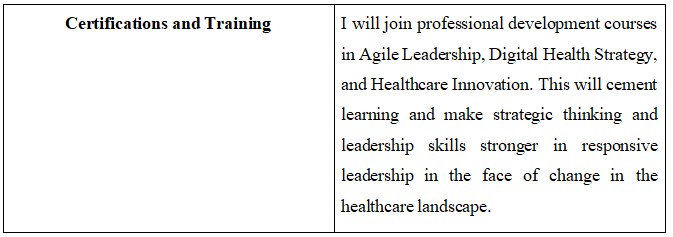
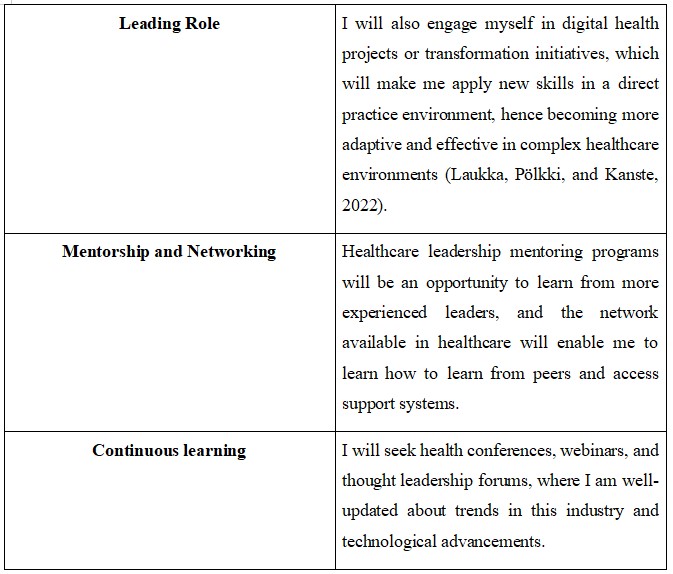
This action plan will continue to help me develop the competencies needed to continue to succeed in healthcare leadership; that is, being ready for whatever opportunities may come up in areas related to digital health transformation or strategic industry positions.
Are you struggling to keep up with the demands of your academic journey? Don't worry, we've got your back!
Exam Question Bank is your trusted partner in achieving academic excellence for all kind of technical and non-technical subjects. Our comprehensive range of academic services is designed to cater to students at every level. Whether you're a high school student, a college undergraduate, or pursuing advanced studies, we have the expertise and resources to support you.
To connect with expert and ask your query click here Exam Question Bank

