Integrated Approaches to Mental Health and Substance Abuse in Critical Nursing Practice NUR4605
Introduction
Nursing incorporates the art and science of providing care and emphasises the protection, promotion and optimisation of health care for people seeking critical care. It can help improve human functioning while also enhancing the avoidance of illness and injury by facilitating proper health care and mitigating suffering through sympathetic presence. This study has been based on identifying such clinical issues of substance abuse and mental health based on which specific strategies can be reflected to bring certain improvements in special practice (Chua et al., 2023). The main aim of nursing is to provide proper care to healthcare seekers distressed by mental health problems or any other behavioural issues. Such task performance by mental healthcare seekers can be similar to that of specialised treatment that they can get. This has been used in identifying such clinical issues of substance abuse and mental health, from which it was possible to reflect on certain strategies that can be used to bring about certain improvements in special practice (Chua et al., 2023). In order to reflect on these issues and enhance practice, a framework by Gibbs (1988) will be suitable. The strengths of this model include the ability to make the practitioners break down their experiential learning systematically to achieve better lessons in their future practice. The main focus of nursing is to ensure that medical patients who attend health facilities with mental-related disorders or any behavioural complications are well attended to.
Identification of clinical issues or situations that require improvement
Substance abuse and mental health issues are related to the challenges or barriers in accessing the proper healthcare services provided in specialised care. It has been taking a crushing toll on the people who might seek advanced nursing care and treatment but might be failing to achieve it (Jarrad et al., 2018). For instance, the pandemic has acted as a catalyst to increase the number of cases related to substance abuse and mental health issues for people across ages and diverse backgrounds. Despite the increasing number, the amount of specialised care people can get is behind the demand. In my opinion, specialising in critical care is not just to develop care plans but also to ensure people can get the required care. For this, just acknowledging the issue is not enough. Rather, the barriers are to be broken to help the people. I believe that the major problem is mostly associated with cost, which prevents the majority of care seekers from actually getting care (Crowley et al., 2015).
It has been found that 37% and 31% of the cases globally prevent mental health and substance abuse care which is one of the biggest challenges. Followed by that the inability to gain a convenient location to seek healthcare services makes up 28% and 22% since people in rural areas are completely ignored (Woodrow, 2018). Apart from that, the inability to find a specialised care provider makes for 25% of mental health care seekers and 31% of substance abuse care seekers, respectively. Also, the remaining people have to endure long waiting hours, which also prevents them from gettingproper care. Overall, such issues need to be resolved, and the situation needs to be improved (Egerod et al., 2021). Based on these issues, I will develop some strategies that might help people across the world from diverse socio-economic backgrounds.
Critical review of the topic
As opined by Gullick et al., (2019), substance Abuse is considered a disorder but is a treatable mental problem that can impact the behaviour and nervous system of an individual while leading them to become unable to switch their use of substances such as legal, and illegal drugs, alcohol or even other types of medication. The symptoms of the clinical issues can be moderate to fatal depending on the level of addiction being the most severe in terms of substance abuse. Some of the common risk issues can donate to both substance abuse and mental problems, which can run in families, which means some genes can be a significant risk factor. Apart from that, environmental factors such as stress and trauma can also be a reason for the genetic alterations passed down through the bloodline. According to Weare et al.(2019), it may consider the development of a mental illness and substance abuse, while it can also be said that mental health issues can contribute to substance abuse in people. Several studies also show that persons with mental health issues such as depression, anxiety or post-traumatic disorder might use drugs and alcohol as to form of self-medication. In some cases, drugs might provisionally help with certain indications of mental health problems. This might make the indicators worse over time, and the brain can change in persons with mental problems, which might increase the rewarding impact of substances. Overall it can make it more likely that a person can continue abusing substances that they might be addicted to.
Service in the context of prevention and treatment of substance abuse might have been traditionally delivered separately in the case of mental healthcare seekers and general healthcare seekers. Due to this, substance abuse has conventionally been considered as a social issue, and inhibition services are not typically developed as an accountability of healthcare systems (Sevilla Guerra et al., 2022). For this reason, people who need care in case of substance had access to only a certain variety of treatment choices that are generally not even covered under any type of insurance. As stated by Mahmoud et al., (2024), efficient integration of prevention, treatment and recovery of services across the healthcare systems can be a major key to addressing the issue of substance abuse and mental health problems along with the consequences that might represent the most promising methods to enhance access based on the quality of treatment. It has been said that in current healthcare laws, certain reforms are made as well as a wide range of other trends in terms of the healthcare arena for facilitating higher standards of addition to better serve people and public health while reducing the disparities in treatment and also reducing the cost towards the society.
As per the views of Molina-Mula et al., (2018), healthcare-based institutions such as health homes or other responsible care organisations are being industrialised to provide more integrated care. The role of the prevalent care delivery organisation, such as community-based health centres, might also require to be expanded to meet the demands of integrated care for substance abuse and prevention, treatment and recovery as well. Even now, there are healthcare care experts who constantly hesitate to provide care seekers with medication-assisted treatment (MAT), specifically the medication required for maintenance, such as (methadone and buprenorphine) in case of the opioid abusers since they might be deeply associated owing to erroneous misconceptions related to the treatments such as the ideas they can substitute one form of addiction for another (Elias & Day, 2020). This has completely hindered the implementation of effective methods of medication even by substance abuse, treatment facilities and when they might use the substance abuse treatment providers as they are mostly prescribed at insufficient amounts for insufficient periods. This contributes to the treatment failure and again reinforces a belief that they actually might not be efficient. The required research shows that when used properly. MAT has the potential to reduce or eliminate illicit drug use associated with criminality and infectious disease transfer while restoring the care seekers towards the path of recovery and healthy functioning as well.
According to Almarhabi et al., (2023), behavioural healthcare might include care for the healthcare seekers around mental health and substance abuse while dealing with surrounding conditions, health behaviour change, life stresses and crises along with any other stress-inducing symptoms. Mental health issues and substance abuse alone can be estimated to surpass all physical problems as a major reason for global disability by the year 2020. The studies assess that the significance of healthcare system needs to effectively address behaviour health conditions. In recent times, there has been a call for the implementation of a primary care delivery platform and the related healthcare seeker-centred medical home methods to effectively address such conditions. As stated by Wood et al., (2018), it shows that several individuals are experiencing the outcomes of behavioural health conditions, this includes mental health problems and substance abuse associated with lifestyle problems as well. Such scenarios can also be interlinked to increase the chance of physical health problems, higher rates of mortality, worse treatment results and higher costs of healthcare.
According to Delaney & Vanderhoef (2019), the higher priority in the case of prevention research and development is to comprehend better and target risk factors to develop protective measures. This might include the investment in potential cohort studies to understand how some of the factors can impact rates of mental and substance abuse while investing in long-term outcomes, showing the studies to know if the prevention programs truly prevent or just delay the onset of disorders. It also helps to examine the role and impact of a broader range of disorder-specific and trans-diagnostic risks to help with protective factors across various developmental phases and stages of life. Again, evaluating and refining the prevention line-ups in the real world is also a prioritywith a higher focus on innovation, agility, scalability and constant improvement. It also shows the importance of investment in higher-quality translation research and ongoing evaluation (Nordfjrn et al., 2022).
Reflection model or theory that is used in the plan
Action Plan
Recommended strategies to improve the speciality practice
An integrated system can help in prevention, early interventions, treatments and then final retrieval that can help to address the full range of substance abuse related to health issues which is a logical and required transformation that the society must make to avert any substance abuse. The results might help to meet the requirements of people with substance abuse and it can also help to provide services to people with mild and moderate substance abuse by far the largest part of all the identified in general healthcare facilities. It is likely to decrease the need for critical care and costly substance abuse treatment methods later even though speciality care is still required for people with some major substance abuse (Fernandes et al., 2018). It is for the healthcare workers with other severe health issues and conditions that trigger their mental health problems and add on in the complications. If any individual is suffering from substance abuse and mental health issues it is mostly effective to deal with both the issues at once rather than one after the other.
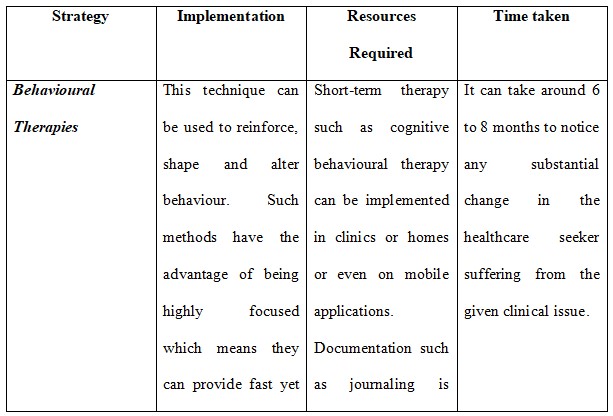
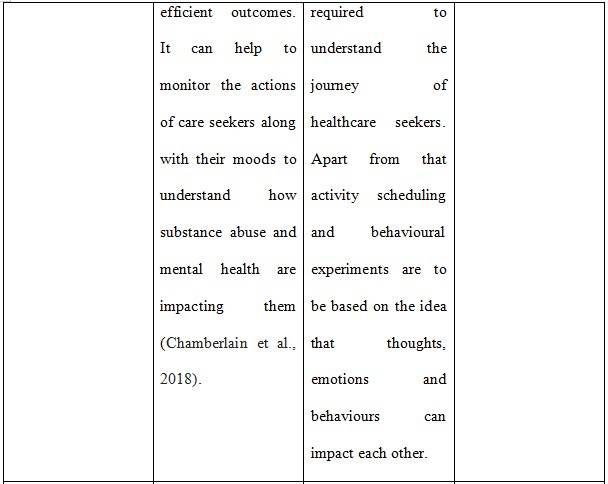
People who might seek help for substance abuse and mental health issues might see a specialist for each disorder and it can be an issue to provide accurate diagnosis since the symptoms can be interdependent. Apart from that it can also add in the cost which can impact the overall treatment process. For this reason, the provider might need to use comprehensive assessment tools to reduce the chance of a missed diagnosis and provide the proper treatment process (Brimblecombe & Nolan, 2021). The specialists must provide tailor-made treatment which might include behavioural therapies and medications as well to a person's specific combination of disorder and symptoms. It should also take into account the age of the person, the type of substance that can be used and the specific mental disorder they are suffering from. Communication with the specialist and healthcare seekers might also help to understand the treatment as it might be more efficient for the individual and provide the treatment sufficient time to make some substantial changes (Barr et al., 2019).
Medication-assisted treatment is the implementation of medication in combination with counselling and behavioural therapies for the treatment of substance use disorder. For those with an opioid use disorder (OUD), medication addresses the physical challenges that one might experience when they stop taking opioids (Teece et al., 2020). Cognitive behavioural therapy is a common therapy used in a substance use order treatment plan. Such an approach can help people identify and change unhelpful trends of thoughts that contribute to their substance abuse. It provides strategies to manage triggers and requirements while it can also provide skills which can be used to cope with stress along with other negative emotions.
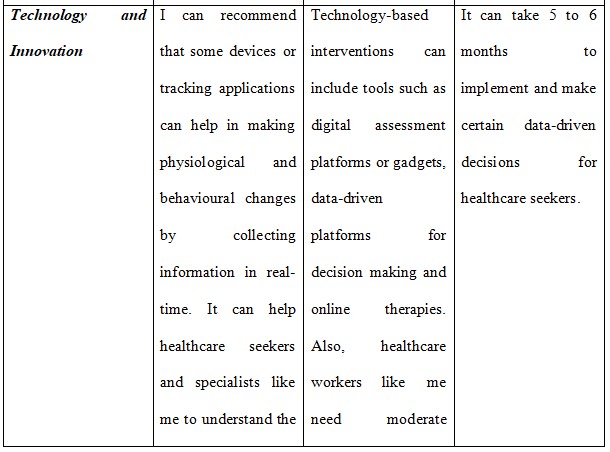
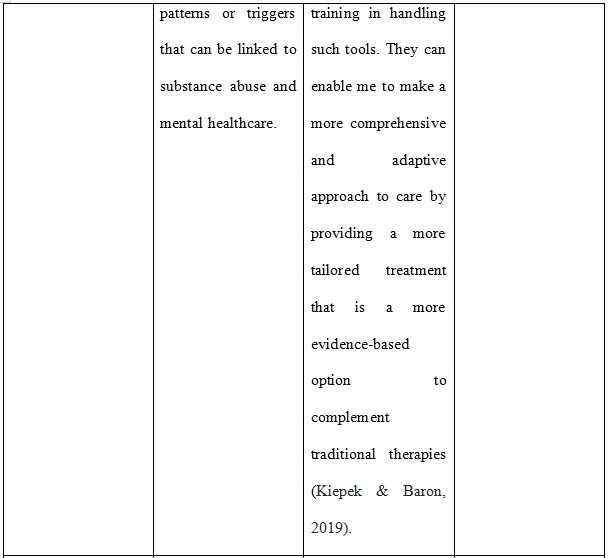
Some of the primary aims of CBT are to help bring awareness correct maladaptive behavioural patterns, and enhance motivation along with change while also developing healthy coping skills. All of these can be beneficial in substance abuse treatment and CBT addresses violence as a learned behaviour and attempts to alter that behaviour. Some CBT programmes might also consider emotional components of domestic abuse such as empathy and might not only be behavioural in their approach (van Schijndel et al., 2022). It might review three major uses of technology to support the treatment of substance abuse health issues such as telehealth, remote, biometric monitoring and digital health interventions. Such technologies can use telecommunication technology such as two-way interactive video to provide services to healthcare seekers with substance abuse from a distance (Raaj et al., 2023).
Conclusion
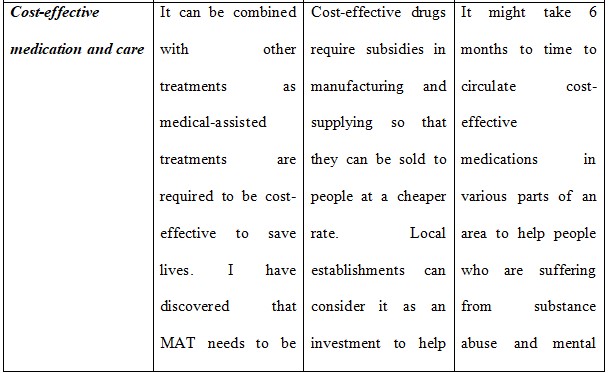
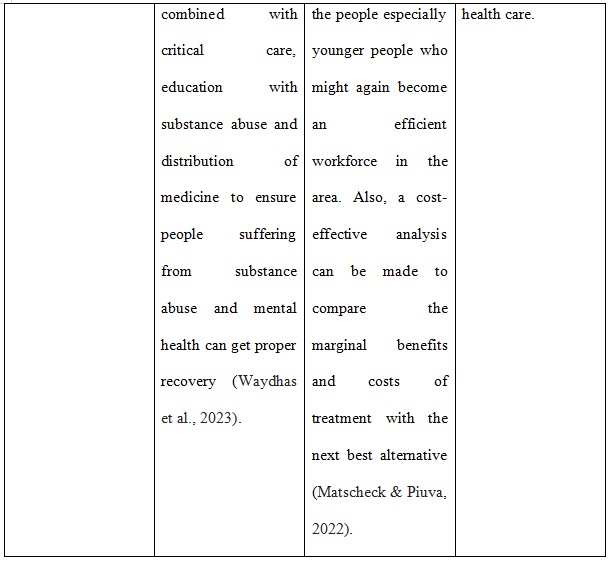
From the study, I can conclude that medical-assisted treatment, cognitive behavioural treatment and cost-effective medication can be integrated with critical care to ensure that proper help can be provided for people suffering from substance abuse and mental health issues. The main issue is the lack of cost-effectiveness of such treatment and the stereotyping of people who might suffer from such types of health problems. People who belong to lower socio-economic backgrounds are more prone to such illness but such people are not able to access the treatment plan due to certain issues. Lack of proper treatment facilities is also a reason, according to me, due to which proper care is not provided to the people who might need intensive care.
Are you struggling to keep up with the demands of your academic journey? Don't worry, we've got your back!
Exam Question Bank is your trusted partner in achieving academic excellence for all kind of technical and non-technical subjects. Our comprehensive range of academic services is designed to cater to students at every level. Whether you're a high school student, a college undergraduate, or pursuing advanced studies, we have the expertise and resources to support you.
To connect with expert and ask your query click here Exam Question Bank

